Vein Treatments
New York & New Jersey

Vein Treatment Overview
“Each patient has to be evaluated individually to establish a vein treatment plan tailored to the individual patient using the best combinations possible as proven by our experience and current guidelines.”
Introduction
For the past decade, our vein centers have been successful at growing into one of the best vein clinics in New Jersey and New York. With unparalleled experience and skill, our vein doctors have been consistently recognized by our patients, peers and institutional societies for high level patient-centered care. treatment.
This guide provides insight into the best practices for spider and varicose vein treatment. It summarizes key up to date literature on vein treatment and our own experience in treating patients. Interested patients can use this guide to advance their knowledge on vein disease and make the best decisions on their vein treatment.
Patient Centered Approach to Vein Treatment
The Vein Specialist Centers emphasizes the importance of advancing its patient’s quality of life through the treatment of spider veins and varicose veins. Varicose veins are extremely common, affecting up to 75% of women and up to 50% of men.[1] While varicose veins can be unsightly, patients who suffer from this condition, as it progresses over time, are not only concerned about their appearance but also experience significant symptoms from varicose veins.
To that end, our vein doctors rely on objective tools to identify appropriate candidates for vein treatment. This includes the Clinical, Etiology, Anatomy, and Pathophysiology (CEAP) Classification of Venous Disorders and the Venous Clinical Severity Score (VCSS).[2-5]
However, VCSS and CEAP characterize patients primarily by the physical appearances of vein disease rather than the patient’s perspective on symptoms. As such, these tools underestimate the impact of vein disease on patients leading to undertreatment.
In the early stages, varicose veins can have mild symptoms that are even overlooked. Misdiagnosis is common with many patients referred for pain management or orthopedic evaluation. Progression is common and typically leads to severe and largely irreversible problems of chronic venous insufficiency (CVI) captured by traditional classification methods like the CEAP Score. We understand our patients seek out care for varicose veins because of symptoms and the disruption to their quality of life. The primary goal of treatment at the Vein Specialist Centers is to accurately assess patient symptoms and prevent progression to severe disease.
Vein Specialist Centers Method
Symptoms most important to most patients suffering from spider and varicose veins have been identified as heaviness, achiness, swelling, throbbing, and itching (HASTI). These symptoms can present differently for each patient including pain, restless legs, edema and is individual to each patient. To establish the effectiveness of our treatments, we monitor clinical responses to medically necessary treatments using patient-centered scoring. Specifically, VVSympQ captures the patient experience of HASTI ™ symptoms related to chronic venous insufficiency (varicose veins). You can calculate your symptoms using its simple varicose veins questionnaire.
The VVSymQ instrument is a five-item PRO instrument specifically developed in accordance with the FDA Guidance for PROs, to evaluate varicose vein symptoms from the patient’s perspective. Results from two randomized,[6] controlled phase 3 clinical studies using the VVSymQ® instrument demonstrated high rates of compliance with the tool and excellent sensitivity of the test to detect change, and indicated that a reduction in score with treatment was clinically meaningful to patients. These findings provide evidence that the VVSymQ® score is an effective tool for measuring pre-treatment symptoms and demonstrating treatment success.
How Patient Satisfaction Scores Improve Varicose Vein Treatment
Having a successful vein clinic relies on a high level of patient satisfaction. We have used our experience monitoring patient outcomes with vein treatment to now appropriately select patients for individualized treatments. To understand the effects of treatment, it is important to understand each patient’s baseline experience of symptoms and impact on quality of life. These symptoms are then followed closely during and after treatment. Symptoms vary among patients, and some treatment effects are not well observed on physical exams or ultrasound. The most meaningful results are best measured using patient-reported outcomes after vein treatment. In other words, to more completely understand patients with varicose veins, we evaluate symptoms before and after treatment. By expanding our definition of success to include assessment of patient response to treatment (in addition to disease severity scores and post-treatment ultrasound findings), we have improved the experience of our patients.

Our Vein Clinics Analysis
The VVSymQ® instrument is a validated tool for evaluating varicose veins based on patient experience. Our vein centers have successfully used this patient-centered approach for identifying the right candidates for vein treatment and continuous monitoring.
Similar Procedures: Endovenous Laser Vein Ablation (EVLA)
Varicose Vein Treatment:
Endovenous Radiofrequency Vein Ablation (EVRFA)
By Dr. Faisal Siddiqi
Introduction
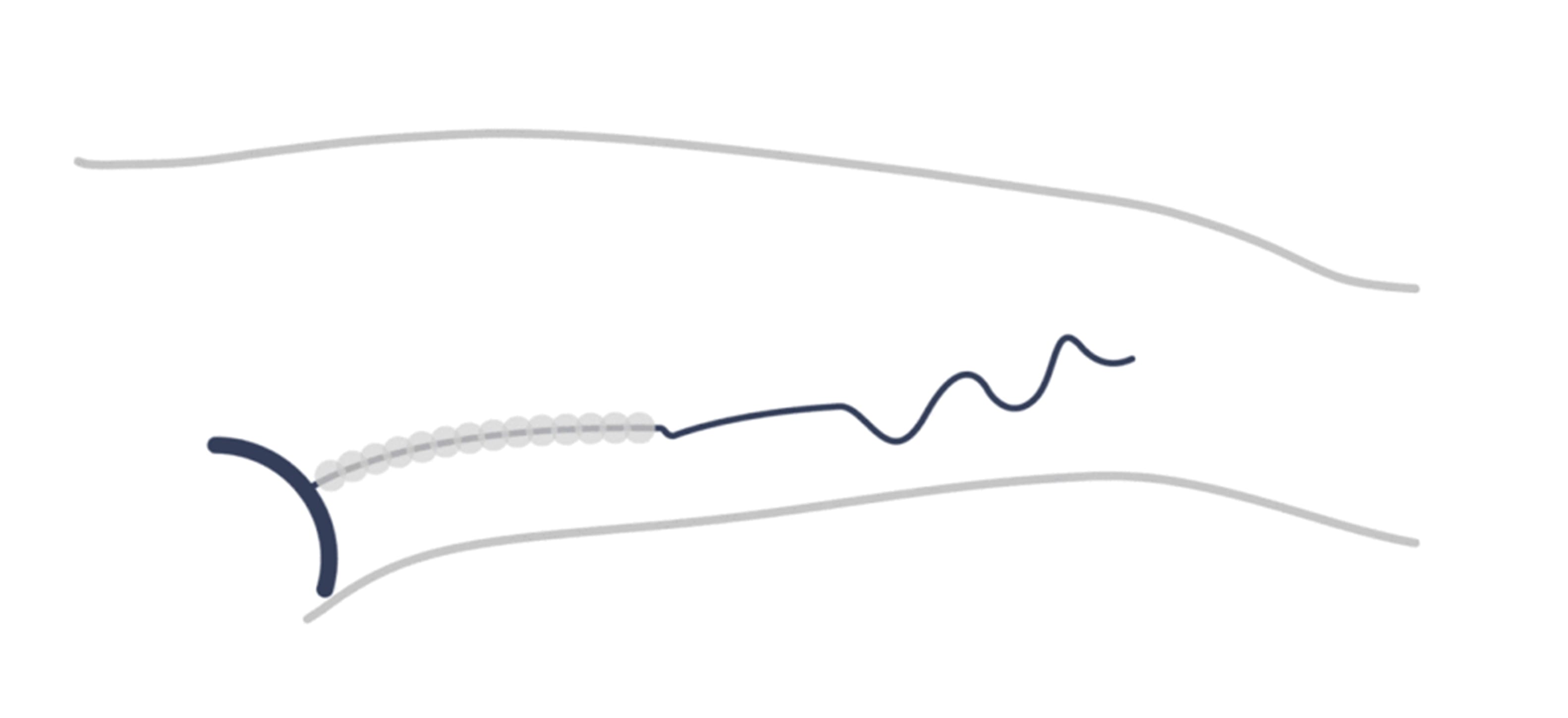
Radiofrequency ablation is a minimally invasive treatment for varicose veins. During ablation, thermal energy is used to heat tissue and create scars that collapse unhealthy veins. This technique uses radiofrequency energy (instead of laser energy) to heat up and damage the wall inside a vein. RF vein ablation is now the gold-standard of varicose vein treatment replacing surgical stripping. To treat a varicose vein, radiofrequency energy is applied from a small catheter inserted through a leg vein.
The procedure is simple and effectively done in the office. A thin catheter is inserted into the target feeder vein using ultrasound guidance and a small IV line. Once the catheter is accurately positioned, the surrounding area is given a local anesthetic solution (tumescence). The catheter is then activated to deliver radiofrequency (RF) energy to the vein wall. The radiofrequency heats and ultimately collapses the diseased vein.
In the past, patients often found "vein stripping" to be a challenging procedure involving the removal of the entire saphenous vein through large skin incisions. However, with the current endovenous techniques, there is no longer a need for skin incisions or anesthesia to treat varicose veins.
Most highly skilled vein specialists can do this with a simple needle puncture under local anesthesia. It can be done in an office setting or ambulatory surgical center (ASC) and the entire procedure can take 30 minutes in skilled hands. You will be able to resume your normal activities shortly after the treatment. After treatment, you will wear compression stockings until your follow-up with the treating doctor. An ultrasound is performed at the follow up visit to ensure adequate treatment.
Is it Safe?
An experienced vein specialist can safely perform an ablation with minimal risks. Possible side effects of radiofrequency ablation include:
- Skin burn (rare)
- Nerve irritation or skin sensory disturbance (usually temporary)
- Phlebitis
- DVT (rare with a trained vascular doctor)
These side effects are rare and should be discussed ahead of time with your vein specialist.

How Well Does it Work?
Radiofrequency ablation is the gold standard for treating venous insufficiency and has a success rate equal to 95%.
In the rare instances, a vein does not collapse with vein ablation, repeat treatment can be offered versus an alternative treatment like VenaSeal or foam sclerotherapy.
What Are The Benefits of RF Vein Ablation?
- Gold-standard of vein disease treatment for underlying venous insufficiency
- Local Anesthesia only
- No downtime, No sutures, No scars
Covered by medical insurance for medical necessity
Limitations of RF Vein Ablation
- RF vein ablation is not intended for spider veins or visible veins directly on the surface.
- Sclerotherapy is often performed in conjunction with RF vein ablation to target large varicose veins on the skin and spider veins.
Do Varicose Veins Recur?
The simple answer is yes. However, there are many contributing factors to the development of recurrent varicose veins.
- New sites of venous insufficiency
- Incomplete treatment of varicose veins
- Incomplete preoperative planning
- Perforator disease
Despite many years of experience, there is still a disappointingly high rate of varicose vein recurrences. Being selective about your vein doctor and having a complete examination before treatment is critically important towards minimizing risks of recurrences. Inadequate investigation before vein treatment and high rates of recurrences are linked to inexperienced vein clinics. The vein doctor must have accurate information using duplex ultrasound to identify all sites of incompetence to plan successful individualized treatments.
Questions to Consider Before Vein Ablation
- How much does the exam and treatment cost?
- How many treatments does the doctor think you will need?
- What are the risks of each specific vein treatment?
- What are the expected results of varicose vein treatment, and how soon can you see symptomatic improvement?
- What are my alternative options for vein ablation?
Physician's Synopsis
- Vein Ablation is the gold standard for the treatment of venous insufficiency
- Vein Ablation is minimally invasive and can be performed with local anesthetic
- Recurrence rates can be unacceptably high with inexperience vein centers
- Complete ultrasound examination and interpretation are critically important to planning successful vein treatments
Similar Procedures: Medical Adhesive, Venous Glue VenaSeal Vein Glue By Dr. Simon Smith
Introduction
The most recent innovation in the treatment of varicose veins is VenaSeal, otherwise known as vein glue.
The VenaSeal closure system uses an advanced medical adhesive that closes the diseased vein. It is the only non-thermal, non-tumescent, non-sclerosant procedure approved for use in the U.S., which means no heat and no swelling.
VenaSeal is developed by Medtronic and used to seal saphenous veins in the thigh or calf region. Once the vein has been treated, it will harden and gradually be absorbed by the body. The procedure is minimally invasive similar to endovenous vein ablation.
It is a non-thermal, non-tumescent curative procedure used to treat varicose veins. It is equally effective as endovenous ablation but without heat or tumescent anesthesia. Instead, VenaSeal involves the injection of a medical adhesive into the affected vein, sealing it shut and redirecting blood flow to healthy veins. This minimally invasive procedure requires no compression stockings post-treatment and has a fast recovery time. VenaSeal is a safe and effective alternative to traditional vein stripping surgery, with a high success rate and patient satisfaction.
How Does VenaSeal Work?
The VenaSeal procedure involves the percutaneous placement of a small catheter through the skin using minimally invasive techniques. In place of heat energy, the catheter delivers small amounts of vein glue to the targeted segments of the saphenous vein under ultrasound guidance. Once the affected vein is closed, blood is immediately re-routed through other healthy veins in the leg. Because VenaSeal does not use any heat energy, there is minimal need for even local anesthesia during the procedure. Stockings are usually not necessary after VenaSeal treatment. This provides added comfort for patients and allows them to return to normal activities sooner.
How Effective is the VenaSeal Procedure?
The published success of the VenaSeal closure procedure is equal to other endovenous procedures, including laser ablation (EVLA).
VenaSeal has been independently studied in the United States and Europe over the last decade. In addition to effective treatment of saphenous veins, published results show a low risk of complications.
What is VenaSeal Made of?
VenaSeal is a treatment that involves the implant of cyanoacrylate, a medical-grade glue. It is a quick, minimally invasive procedure that takes approximately 30 minutes in experienced hands.
Interesting properties of VenaSeal that make it particularly useful in vein treatment include:
- It rapidly polymerizes on contact with blood resulting in an immediate effect on the vein walls.
- The glue displaces the blood inside the vein and seals the walls shut. As a result, compression stockings are not required after vein treatment.
- Has an “anti-microbial” effect against bacteria on the skin.
Physician's Synopsis
Advantages of VenaSeal
- Treatment is performed without any delivery of heat energy eliminating the risk of injury to skin or nerves
- Increased comfort for procedure versus traditional surgery and endovenous ablation
- No need for compression stockings after vein treatment
- Quick recovery with no downtime
Disadvantages of VenaSeal
- Small, rare intolerance to the adhesive
- Implant lacks long-term data for efficacy
- VenaSeal has limited insurance coverage at this time
Similar Procedures: Cosmetic Sclerotherapy, Cryosclerotherapy, Liquid Sclerotherapy Sclerotherapy By Dr. Claudia Rios-Datta
Introduction
The gold standard treatment of spider veins is sclerotherapy, which can treat a large variety of small and large veins. Laser vein removal is limited to facial veins or very fine veins on the legs or particularly feet.
Sclerotherapy is used to treat and remove spider veins and varicose veins on the legs, ankles, and feet. Sclerotherapy can also be used for some facial veins, breast veins, and hand veins.
An FDA-approved medicine called Asclera™ or polidocanol is injected into the vein using a fine needle. The vein becomes irritated from the solution, causing it to collapse and absorb into the body. The procedure can be done in the office and is suitable for many types of veins.
What is Sclerotherapy?
Sclerotherapy involves the injection of a medicated solution, called a sclerosant, into spider veins. The sclerosant irritates the lining of the blood vessels and causes them to collapse. Over subsequent weeks and months, the body gradually absorbs the vein. Each treatment can be associated with 50-60% improvement, with multiple treatments required for 80-90% improvement.
Sclerotherapy can be augmented with several advanced techniques, including:
- Ultrasound-guided sclerotherapy
- Veinlite enhanced sclerotherapy
- Augmented Reality
Cryosclerotherapy is an additional measure to enhance patient comfort. The whole procedure is done using a cryo unit that produces a continuous flow of cold air to the sites of application of sclerotherapy injections. The result is the cold air anesthetizes the skin, so the treatment is relatively painless. This is especially helpful for the treatment of spider veins in sensitive areas like the behind the knees and thighs.
What to Expect from Sclerotherapy
- All patients with spider veins are assessed for underlying venous insufficiency. In some instances, a reflux ultrasound may be requested by your vein specialist to identify any abnormal veins beneath the skin contributing to symptoms and spider veins.
- Any underlying venous insufficiency is considered for vein treatment prior to sclerotherapy.
- Foam sclerotherapy is often reserved for large surface varicose veins or patients with residual vein disease from prior vein treatment.
- The most effective sclerosants include polidocanol and sodium tetradecyl sulfate (STS). Hypertonic saline is an older technique associated with increased risks for hyperpigmentation and skin injury.
- The concentration of sclerotherapy is planned by your vein specialist based on the size of target veins.
Instructions Prior to Sclerotherapy
- Your usual medications can be continued prior to treatment (hormonal therapy, birth control, iron supplementation should be discussed ahead of time)
- Do not apply lotions on the day of treatment
- Do not shave your legs immediately prior to your treatment
- Any travel plans should be discussed ahead of time with your physician
- Patients who smoke should consider stopping before any treatment
Sclerotherapy Treatment Options
Sclerotherapy treatment for spider and varicose veins is tailored to each patient’s condition. Our vein doctors will select the right preparation of sclerotherapy based on the severity of your vein disease and how you want to treat your spider veins.
Liquid Sclerotherapy
This is the most basic form of sclerotherapy treatment and involves direct injections of the liquid solution into the affected veins. This form is best suited for smaller spider veins, as it is minimally invasive and requires no downtime. The liquid solution causes the veins to shrink and eventually disappear, resulting in smoother, clearer skin.
Foam Sclerotherapy
During this treatment, small amounts of liquid solution are mixed with air to create a foamy, cream-like substance. This allows for greater activity against the diseased veins. Foam sclerotherapy is 5x as potent as liquid sclerotherapy and an effective treatment for treating slightly larger feeder veins and venulectasias.
Ultrasound-Guided Sclerotherapy
For varicose veins that are difficult to see, as well as large superficial veins, ultrasound-guided sclerotherapy can improve precision and accuracy where other techniques cannot. This technique requires more patience and skill on the vein doctor’s part. Vein Specialist Centers has American Registry for Diagnostic Medical Sonography (ARDMS) certified technicians and physicians to successfully perform ultrasound-guided sclerotherapy techniques. ARDMS is the recognized standard for excellence in ultrasound.
What Happens During Sclerotherapy?
- Understandably, some patients are anxious about spider vein treatment and needle pricks. We can assure you that most patients have very little discomfort from sclerotherapy.
- A typical procedure lasts between 15 minutes to 30 minutes
- Multiple sessions may be planned depending on the condition of your veins
- Larger veins are addressed first down to the smaller veins
- Specialized equipment, including vein-lites, magnification, and cooling techniques, may be utilized
- A topical steroid can be immediately applied post-treatment for any skin irritation at the discretion of the vein doctor.

After Treatment
Following each treatment session, patients may benefit from compression stockings. Sun exposure after treatment should be avoided for at least four weeks or until bruising has subsided. Read more about sclerotherapy aftercare.
What Are the Possible Complications of Sclerotherapy?
Deep vein thrombosis (DVT)
Clots are a recognized complication of vein treatment, however rare in inexperienced vein clinics. Increasing pain or leg swelling after treatment deserves immediate attention.
Allergic reaction
The most common reaction is a skin wheal similar to mosquito bites. No treatment is required. However, topical cortisone may alleviate any itching. More serious reactions are extremely rare and immediately recognized as difficulty breathing or a change in health status. On-site treatment with steroids or epinephrine is required.
Skin ulceration
Skin ulceration or tissue necrosis is another rare complication, especially with newer sclerosants. It occurs mainly because of inadvertent injection into the dermal capillaries and arterioles. In our experience, most injection ulcers are small and will heal without scarring. However, early attention is warranted for optimal resolution.
What Symptoms Can You Expect After Sclerotherapy?
- Mild Discomfort after sclerotherapy is more often related to compression stockings. The stockings can be removed for periods of time to provide some ease.
- Darkening of Spider Veins. Some treated spider veins may darken in the initial weeks after treatment due to trapped blood. This is a sign of successful spider vein treatment, and the area will gradually fade with time.
- Bruising is seen more often with the treatment of larger veins with ablation or phlebectomy.
- Hardened, Lumpy Veins are another sign of successful vein treatment. The hardened veins do not require any further sclerotherapy and will be gradually reabsorbed by the body. Trapped blood can be removed with a few needle pricks.
- Hyperpigmentation represents hemosiderin deposits released from the treated veins. Prevention is the best course of action, using meticulous techniques and the lowest concentration of sclerosant for effective results. Early evacuation of trapped blood is recommended. Most hyperpigmentation resolves spontaneously by 6-12 months.
- Telangiectatic Matting occurs 4-6 weeks after treatment and resolves spontaneously. They appear as tiny, fine new capillaries on the surface of the skin, particularly near injection sites. Spontaneous resolution is expected. However, identification of any larger refluxing veins is recommended. For most patients undergoing cosmetic sclerotherapy, very few symptoms are expected with treatment.
- Phlebitis. Inflammation of the treated veins can occur during the healing process. Redness and tenderness will appear over the treated veins. Treatment goals are comfort provided by compression stockings, warm compresses, and NSAIDs. Regions of associated coagulum can be removed with simple needle drainage.
Physician's Synopsis
- Sclerotherapy is the preferred treatment for spider veins in comparison to laser vein removal
- Several enhanced techniques can enhance the effectiveness of treatment
- Many patients require staged treatments with the expectation of 80-85% improvement
- Side effects are rare
Similar Procedures: Foam Sclerotherapy, Pre-mixed Foam Sclerotherapy Ultrasound Guided Sclerotherapy By Dr. Claudia Rios-Datta
Introduction
Ultrasound-guided sclerotherapy (UGS) is a highly specialized procedure for treating varicose veins that are hidden beneath the skin.
Not all varicose veins are visible and some feed directly into the spider veins on the surface of the skin. In these cases, ultrasound is used to identify the target vein, and the medication is injected into the desired segment. Vein doctors adept at ultrasound techniques are best suited to perform this advanced technique for vein removal.
How Does Ultrasound Guided Sclerotherapy Work?
A detailed ultrasound examination is performed prior to sclerotherapy to create a road map of the lower leg veins. This map precisely displays all abnormal veins and helps the vein doctor identify the root cause of the visible spider veins and varicose veins.
Using ultrasound guidance, the doctor can accurately guide the needle and inject the sub-surface veins underlying visible ones. The ultrasound also helps identify regions of deep venous connections (perforator veins) that are carefully monitored during treatment. Once injected, the treated vessel will collapse and gradually be absorbed by the body, disappearing with time.
Foam sclerotherapy is well visualized on ultrasound and allows for real-time monitoring of treatment. The foam is better suited for larger varicose veins than liquid sclerotherapy as it maintains better contact with the vessel walls. Additional safety enhancements include pre-formulated compounds with O2:CO2 mixtures that micronize bubbles leading to more uniform treatment. In our vein clinic, we routinely perform ultrasound-guided sclerotherapy for large visible varicose veins, neovascularization, and residual segments of saphenous veins that are tortuous or in close proximity to vulnerable structures like skin and nerves. It is used in conjunction with vein ablation for the best results.
What Happens During Ultrasound Guided Sclerotherapy?
- The target vein segments are mapped with ultrasound. Entry sites and perforator veins are marked on the skin for special attention.
- The target vein(s) is accessed using ultrasound guidance, and the sclerosant is injected into the vein
- Foam sclerotherapy is visualized in real-time to monitor treatment response. Additional injections are given based on this information. The leg is often elevated during the injection to increase the treatment response
- Smaller spider veins may be treated during the same session or during follow-up for cosmetic sclerotherapy
What Happens After Treatment?
The treatment usually takes half an hour, with some additional time allotted for ultrasound examination, patient preparation, and discussion. Following the procedure, patients are fitted with grade 2 graduated compression stockings and foam padding. Most routine activities can be immediately resumed after treatment.
Patients return to the vein clinic in one week following the UGS procedure. At this follow-up appointment, a focused ultrasound is performed to ensure that the treatment is successful.
How Effective is Ultrasound Guided Sclerotherapy?
A randomized controlled trial comparing foam sclerotherapy to laser ablation and surgery found that laser ablation and surgery had better outcomes and that laser had the fewest procedural complications. We reserve the use of foam sclerotherapy for necessary adjunctive treatment of saphenous vein segments following vein ablation or prior surgical therapy, large surface varicose veins, and segments of neovascularization. In our practice, vein ablation is the preferred treatment for most vein segments.
What Are the Possible Complications of Sclerotherapy?
Complications can occur even with the best possible technique and attention to detail.
- Deep vein thrombosis (DVT). Clots are a recognized complication of vein treatment. However rare in experienced vein clinics. Increasing pain or leg swelling after treatment deserves immediate attention.
- Allergic reaction. The most common reaction is a skin wheal similar to mosquito bites. No treatment is required. However, topical cortisone may alleviate any itching. More serious reactions are extremely rare and immediately recognized with symptoms of difficulty breathing or change in health status. On-site treatment with steroids or epinephrine is required.
- Skin ulceration or tissue necrosis is another rare complication, especially with newer sclerosants. It occurs mainly because of inadvertent injection into the dermal capillaries and arterioles. In our experience, most injection ulcers are small and will heal without scarring. However, early attention is warranted for optimal resolution.
What Are Common Symptoms After Sclerotherapy?
For most patients undergoing ultrasound-guided sclerotherapy, a few common symptoms can be expected, and it is good to know ahead of time.
- Mild Discomfort can be related to the normal healing process after vein treatment. Our vein clinic will monitor your treatment with an ultrasound one week after the injection.
- Bruising is not uncommon after vein treatment.
- Lumps and bumps are another sign of successful vein treatment. The hardened veins do not require any further sclerotherapy and will be gradually reabsorbed by the body. Trapped blood can be released with needle drainage if appropriate.
- Hyperpigmentation represents hemosiderin deposits released from the treated veins. Prevention is the best course of action, and using meticulous techniques and the lowest concentration of sclerosant is the best way to achieve effective results. Early evacuation of trapped blood is recommended. Most hyperpigmentation resolves spontaneously by 6-12 months.
- Telangiectatic Matting occurs 4-6 weeks after treatment and resolves spontaneously. They appear as tiny, fine new capillaries on the surface of the skin, particularly near injection sites. Spontaneous resolution is expected; however, the identification of any additional refluxing vein segments should be treated.
- Phlebitis. During the healing process, the treated vein segment can become inflamed and tender to the touch. Treatment goals are comfort provided by compression stockings, warm compresses, and NSAIDs. Regions of associated coagulum can be removed with simple needle drainage.
Physician's Synopsis
- Ultrasound-guided sclerotherapy or Foam Sclerotherapy is an effective vein treatment for subsurface varicose veins
- Best used in conjunction with vein ablation
- Reduced risks of injury to skin or nerves
- A smooth and successful procedure is dependent on having a vein specialist experienced in vascular ultrasound technique (RPVI, RVS, or RPhS credentials)
Similar Procedures: Microphlebectomy Ambulatory Phlebectomy By Dr. Claudia Rios
Introduction
Ambulatory Phlebectomy is the surgical removal of bulky, large varicose veins on the skin surface, through tiny incisions. It is a minimally invasive procedure with patients returning to many of their normal activities the following day. Ambulatory phlebectomy should not be confused with vein stripping or surgical stripping procedures. The procedure eliminates varicose veins through a series of tiny incisions directly over the varicose vein segments, removing them in a single setting. Before phlebectomy is performed, any underlying reflux should be identified and treated first with vein ablation or ultrasound-guided sclerotherapy.
- Ambulatory phlebectomy is performed on an outpatient basis under local anesthesia
- The procedure can be performed in 30-60 minutes, depending on the location and severity of varicose veins.
What is the Advantage of Phlebectomy?
Phlebectomies are carefully evaluated against sclerotherapy and are generally reserved for larger veins. While sclerotherapy is more simple, it can be associated with longer recovery periods as it takes time for the veins to absorb. Not all large varicose veins are suited for foam sclerotherapy. Ambulatory phlebectomy is notable for more immediate results and higher levels of patient satisfaction in the right settings.
In our vein clinics, Dr Claudia Rios performs ambulatory phlebectomies in select cases.
Will I Need Stitches?
No, in most instances, the phlebectomy incisions are so small that no stitches are required. For the very same reason, scarring is much less likely. However, certain skin types may be more vulnerable.
Am I A Good Candidate for Ambulatory Phlebectomy?
Ambulatory phlebectomy is a safe and effective therapy for many patients with large visible varicose veins. The procedure is best managed by vein specialists who also routinely perform ultrasound-guided sclerotherapy to weigh the pros and cons of each treatment choice. In some cases, a hybrid approach is appropriate for obtaining the best results.
Do I need Surgery for Varicose Veins?
Absolutely not! Modern spider vein and varicose vein treatments have completely revolutionized. This means no cuts, no sutures, and no downtime. The Vein Specialist Centers utilize cutting-edge tools, including RF vein ablation, VenaSeal, phlebectomy, and advanced sclerotherapy techniques to heal even the most difficult veins. Your vein doctor will customize a treatment plan based on your symptoms and personal goals.
Physician's Synopsis
- Ambulatory Phlebectomy is a useful tool to treat large, bulky varicose veins on the surface of the skin
- Most varicose veins will be treated with a combination of ablation and sclerotherapy
- In our experience, phlebectomy is a reserved tool associated with high patient satisfaction in the right setting
The Future of Vein Treatment Echotherapy
Discover the only non-invasive “vein treatment”: No scars and no incisions.
Treating Varicose Veins Without Surgery
SONOVEIN® is currently available in select European countries after receiving CE-mark approval. It was recently approved by the FDA for clinical trials in the United States.[8] These studies are ongoing and will provide the necessary safety and efficacy data before approval in the US. SONOVEIN® represents the first robotic solution for a 100% non-invasive treatment of varicose veins. Unlike current endovenous procedures, the treatment is performed completely outside the body. There are no catheters, incisions, or post-procedure scars. SONOVEIN® is directly operated by the vein specialist without any significant preparation. Patients can resume their normal daily activities immediately after treatment.
How Echotherapy Works
Vein ablation by echotherapy and radiofrequency have identical tasks – the elimination of source (feeder) veins into symptomatic varicose veins. The main benefit of echotherapy over current therapies available in the US is being completely non-invasive.
The high-intensity ultrasound beam (HIFU) is focused on the vein. A pulse of therapeutic ultrasound is then delivered for a few seconds at the target segments of the diseased vein. As the thermal energy is delivered, the vein shrinks and is sealed closed, similar to other endothermal methods – but non-invasively. Pulses are provided until the complete target area is treated.

Benefits of Echotherapy
- No Scars
- No Incisions
- Immediate Return To Activity
Physician Synopsis
- Exciting New Technology currently being studied and awaits FDA approval
- Offers a completely non-invasive method for varicose vein treatment
- Early experience has been encouraging. However, certain anatomy may not be suitable for HIFU vein treatment
- Adjunctive treatment with ultrasound-guided sclerotherapy will still be useful for large bulky varicose veins and tortuous segments
- Not suitable for spider vein treatment
ClariVein
If you're suffering from unsightly or painful varicose veins or chronic venous insufficiency, ClariVein is a new, minimally-invasive treatment option.
Introduction
ClariVein is a clinically proven and minimally invasive treatment for reducing symptoms of venous insufficiency. It is FDA-approved and non-thermal, meaning no laser is used, and there won't be any scarring. The treatment is completed in less than an hour in our office, similar to other endovenous procedures. ClariVein is an alternative treatment that can complement commonly used procedures like radiofrequency ablation and sclerotherapy. Your vein specialist will assess your current anatomy and previous treatments to determine the best course of action for your specific needs.
The Princeton Vascular Center’s very own vascular surgeon and vein specialist, Dr. Brotman O’Neill, was present for the first ClariVein procedure in the United States and was the first to implement this procedure in Mercer County.
How Is ClariVein Unique?
Unlike EVLT and sclerotherapy, which use a single method to close a damaged vein, ClariVein employs two modes of action to treat both the damaged vein and its underlying cause.
What Happens During a ClariVein Procedure?
The ClariVein procedure involves treating affected veins internally through a small incision typically made on the upper thigh area. Your vein specialist will insert a medical catheter with a rotating fiber into the vein.
After the device reaches the damaged vein, the fiber will initiate rotation, which will remove the lining of the affected vein while also delivering a medical solution to address the underlying cause.
The catheter will rotate for several minutes, and patients may feel a light humming sensation near the affected area. However, it should not cause any significant pain or discomfort.
Is ClariVein Painful?
Like other treatments we offer at Vein Specialist Centers, this procedure is performed with local sedatives in an office-based setting in one of our vein treatment centers. The session can be completed in as little as 30 minutes, and there is very little chance of scarring or bruising since no major incision is made and surrounding tissue is not damaged. After a ClariVein treatment, patients can return to their normal activities almost immediately.
Laser Vein Ablation
Endovenous laser ablation (EVLA), or endovenous laser therapy (EVLT), is a minimally-invasive procedure used to correct an underlying vein disease.
Introduction
Endovenous laser ablation (EVLT) – along with radiofrequency ablation (RFA) – has emerged as the preferred non-surgical technique for treating varicose veins, surpassing traditional surgical stripping. This minimally invasive procedure effectively addresses venous reflux, boasting high long-term success rates. The laser vein ablation procedure is done directly in Vein Specialist Centers’ offices under local anesthesia by the best vascular specialists in New Jersey and New York. Moreover, it leaves no scars, can be completed in under an hour, and allows patients to resume their daily activities immediately after treatment.
How Is EVLA Performed?
Using ultrasound guidance, a laser fiber is carefully inserted into the troublesome vein through a small incision in the skin. Once positioned, the laser emits energy directly into the vein, resulting in its permanent closure. The procedure typically takes less than an hour to complete. Afterward, patients are usually able to drive themselves without assistance.
What Happens After EVLA?
You might be wondering what you can expect after your vein ablation procedure. Once it is complete, the blood is automatically redirected to healthy veins. Leg circulation actually improves immediately after the procedure! After your endovenous laser ablation treatment, walking is encouraged.
Is Laser Vein Ablation Painful?
Luckily, there is no need for any pain medications post-procedure, and most activities can be resumed in a few days. The treatment of venous reflux with EVLT has proven to be highly effective, surpassing the success rates of surgical stripping in the long term.
What Is The Best Vein Treatment For Me?
A consultation with experienced vein specialists at the Vein Specialist Centers will provide insights to help you decide on the best vein treatment plan.
It’s important to have a treatment plan tailored to your specific condition. Varicose veins and spider veins do not fit just one pattern. Conservative measures such as compression stockings and exercise continue to be important tools in treatment. For individuals with persistent symptoms or more advanced disease, minimally invasive treatments are available and preferred.
References
- Beebe-Dimmer JL, Pfeifer JR, Engle JS, et al. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol 2005; 15: 175–184. [PubMed] [Google Scholar]
- Beebe HG, Bergan JJ, Bergqvist D, et al. Classification and grading of chronic venous disease in the lower limbs. A consensus statement. Eur J Vasc Endovasc Surg 1996; 12: 487–492. [PubMed] [Google Scholar]
- Eklöf B, Rutherford RB, Bergan JJ, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. American Venous Forum International Ad Hoc Committee for Revision of the CEAP Classification. J Vasc Surg 2004; 40: 1248–1252. [PubMed] [Google Scholar]
- Vasquez MA, Wang J, Mahathanaruk M, et al. The utility of the Venous Clinical Severity Score in 682 limbs treated by radiofrequency saphenous vein ablation. J Vasc Surg 2007; 45: 1008–1014. [PubMed] [Google Scholar]
- Vasquez MA, Munschauer CE. Venous Clinical Severity Score and quality-of-life assessment tools: application to vein practice. Phlebology 2008; 23: 259–227. [PubMed] [Google Scholar]
- Todd KL, Wright DI, the VANISH-2 Investigators The VANISH-2 study: a randomized, blinded, multicenter study to evaluate the efficacy and safety of polidocanol endovenous microfoam 0.5% and 1.0% compared with placebo for the treatment of saphenofemoral junction incompetence. Phlebology 2014; 29: 608–618. [PubMed] [Google Scholar]
- VANISH-1: Phase III Study of Polidocanol Endovenous Microfoam on the Appearance of Varicose Veins. Podium presentation by Theodore King, Am Coll Phlebology, Florida, November 2012.
- https://echotherapie.com/echotherapy-treatment-by-therapeutic-ultrasounds/
